Rheumatoid Arthritis

Dr. Antoni Chan synovialjoints
3 years 1 month ago
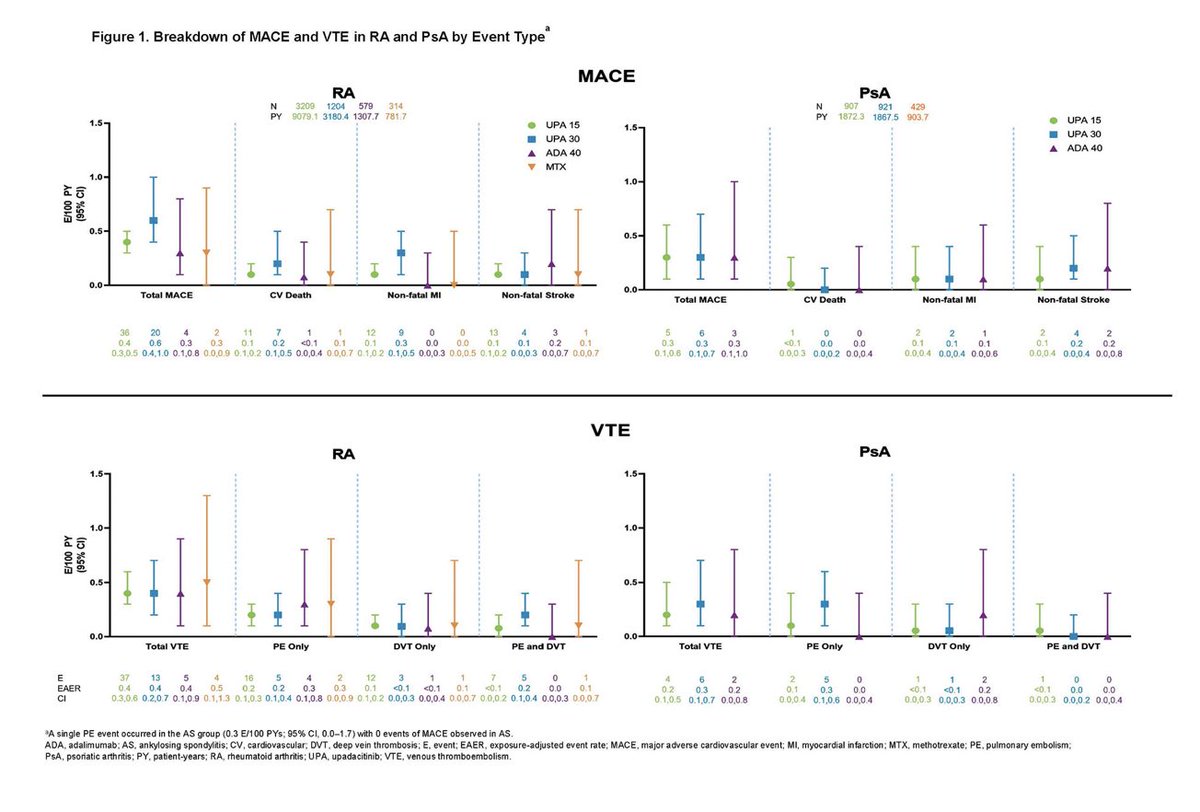
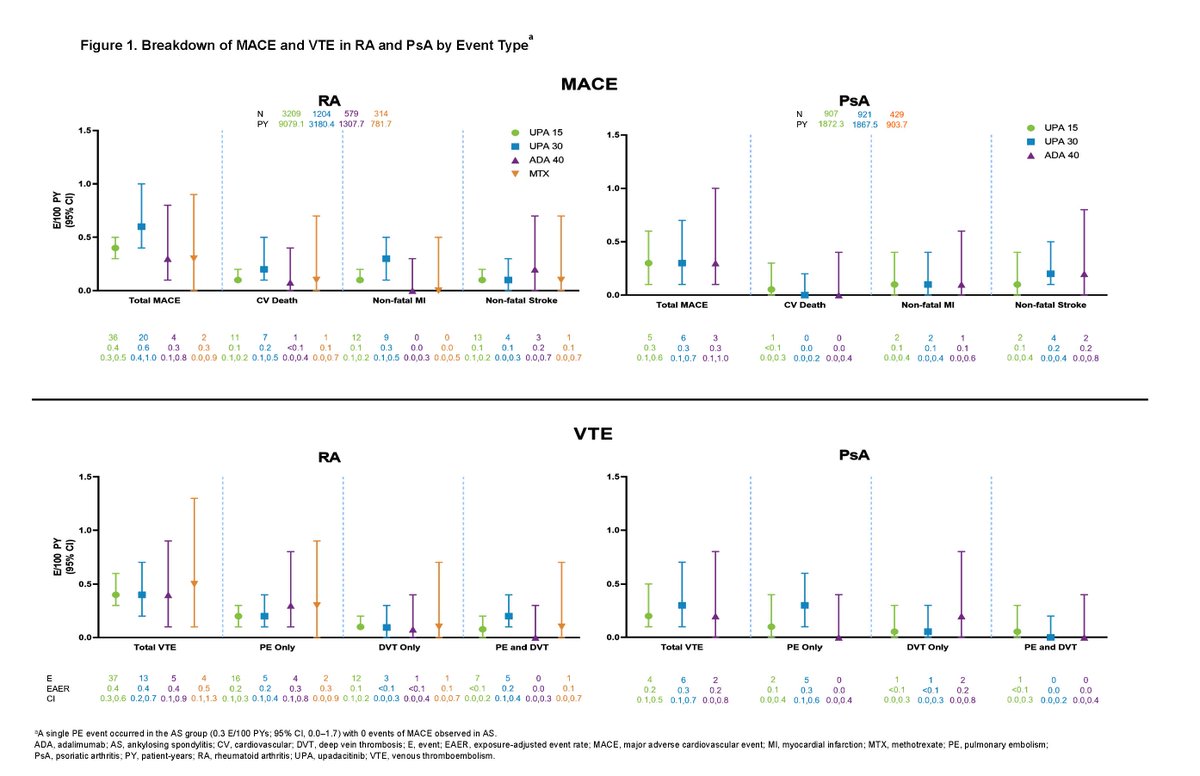
Across 9 trials of Upadacitinib in RA, PsA and AS, 40%–50% of patients had ≥ 2 CV risk factors, ≥ 65 years 6%–23%. Rates of adjudicated MACE and VTE with UPA were infrequent, consistent with background rates in RA, PsA, and AS Abst 0510 https://t.co/HDkQ6ELnAy #ACR22 @RheumNow https://t.co/SRJYdFFNIQ

Catherine Sims, MD DrCassySims
3 years 1 month ago
What has changed since the 2020 @ACRheum #reproductive guidelines?
Abstract #1717 425 SLE/RA patients:
📍 significant improvement in pre-#pregnancy counseling and discussions in reproductive goals
📍No improvements in birth control use or documentation
The RheumNow faculty reporters have been scouring the meeting and online presentations to find the best abstracts from ACR22. Here are some of their choice abstracts reported today on day 1 of ACR 2022 (#ACRbest).

Aurelie Najm AurelieRheumo
3 years 1 month ago
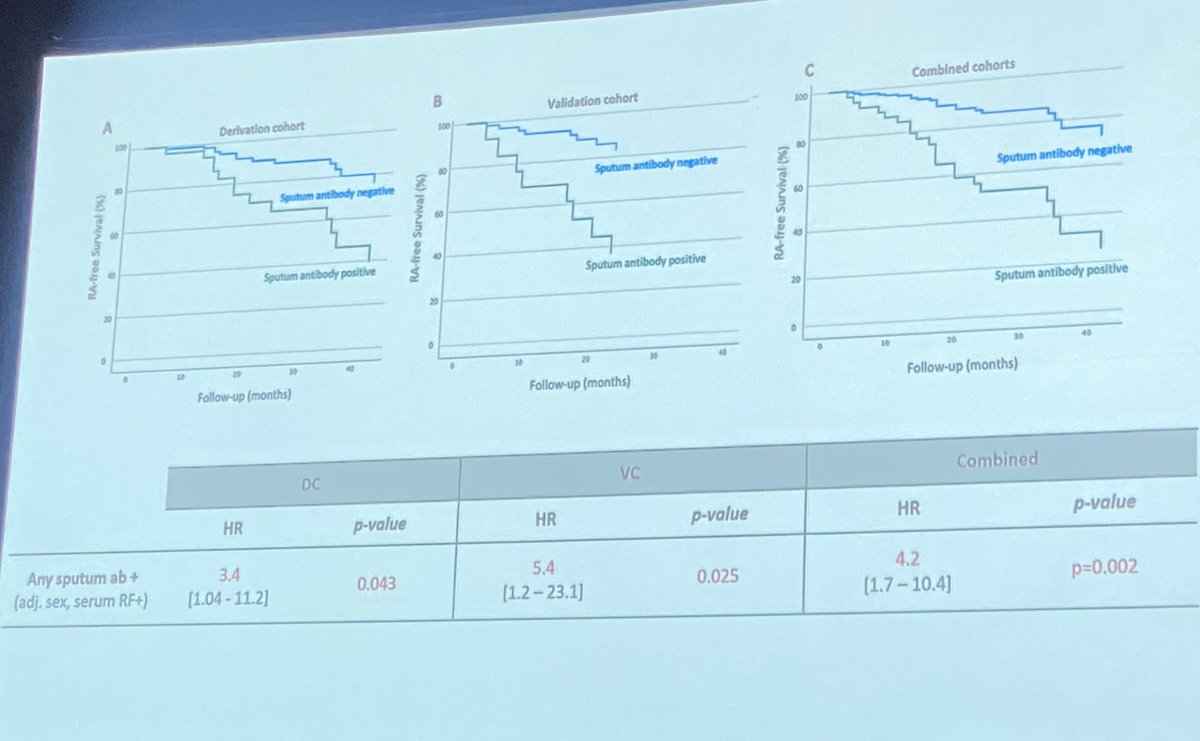
Can we use sputum to identify progression to RA in at-risk individuals?
Sputum anti-CCP-IgA anti-CCP-IgG & RF-IgM positivity = 4-fold increase risk of classified RA in IgG CCP+ at-risk individuals.
Sens 67% Spe 80%
https://t.co/o6PCvxgYGM
Abs #0533 #ACR22 #ACRBest @Rheumnow https://t.co/CxDjanjBKT

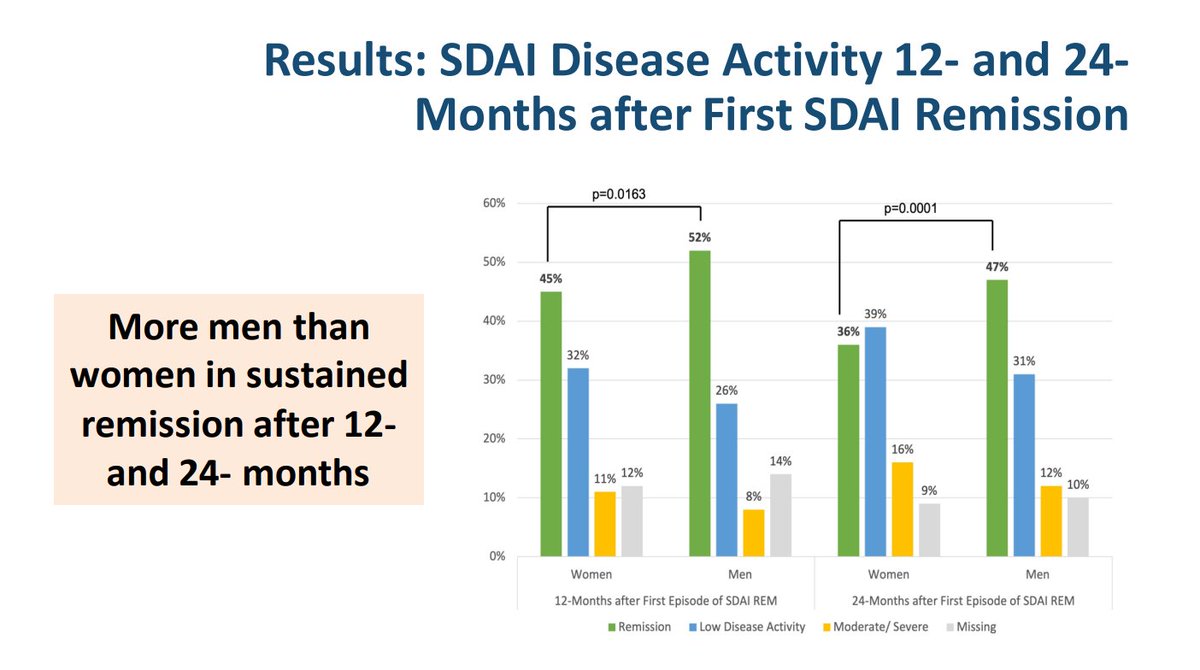
David Liew drdavidliew
3 years 1 month ago
@erasmusmcintl @RheumNow Data here from @earlyarthritis (CATCH Canada cohort), similar results.
It's not just pain differences - but that's real too. It's lots of things, but whatever the case we ignore sex and gender's impact in RA at our peril.
ABST0532 #ACR22 @Janetbirdope @TheLancetRheum @RheumNow https://t.co/27uQmNAlPF
Rheumatoid arthritis is known to be associated with a higher risk of infections. In abstract 0535, Porter and colleagues have assessed infection rates in the pre-RA and early RA phases as defined by antibiotics prescription and hospital admissions with an infection main diagnostic code in the UK National database.

Dr. John Cush RheumNow
3 years 1 month ago
Emerging and exciting treatments in RA: #ACR22 preview
https://t.co/5JtblF9MxE https://t.co/oYSiLguLkJ


Aurelie Najm AurelieRheumo
3 years 1 month ago
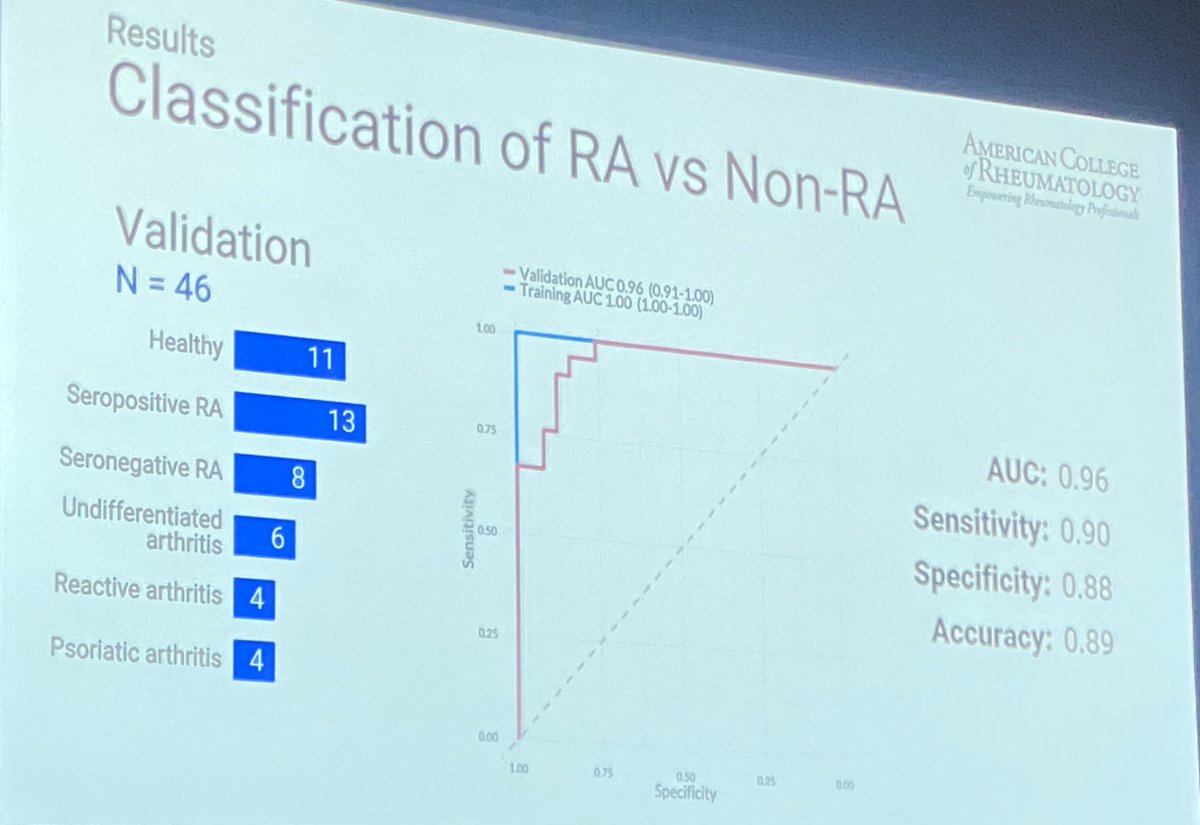
Are DNA methylation marks the new seronegative RA biomarkers?
Riskedal et al. propose a new model based on whole-blood DNAm profiles
Sens 90%, Spe 88%, Accuracy 89% for classification of RA
Accuracy RA Sero+ 100%, RA Sero- 75%
https://t.co/3occAQPZ1u Abs#0531 #ACR22 @Rheumnow https://t.co/QXhMxyWC8g

Aurelie Najm AurelieRheumo
3 years 1 month ago
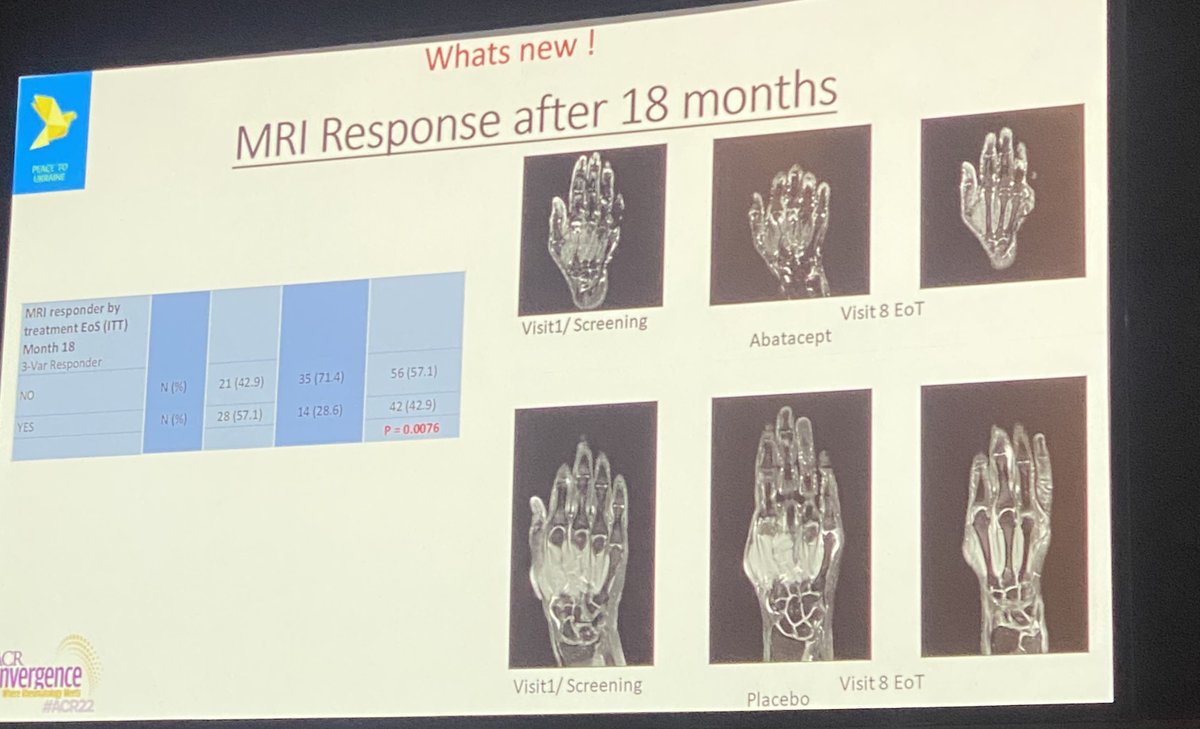
18mo data of ARIAA study (6mo ABA in pre-RA):
12mo after discontinuation
Progression to RA ABA 35% vs PBO 57% p=0.008
Improvement in synovitis, osteitis & tenosynovitis ABA 57% vs. 29% PBO
Enough to move into clinical application?
https://t.co/2CDN9M31mB
Abs#0530 #ACR22 @Rheumnow https://t.co/R54AokGSiK

Robert B Chao, MD doctorRBC
3 years 1 month ago
Rates of MACE and VTE with upadacitinib were infrequent and consistent with background rates in RA, PsA and AS patients. Factors associated with MACE/VTE: age>65, HTN, DM, smoking, history CV event/VTE
Abs#0510 @RheumNow #ACR22 https://t.co/AjtJF0p3QK

Richard Conway RichardPAConway
3 years 1 month ago
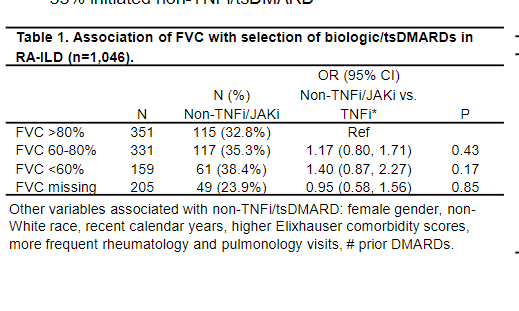
England et al. Influence of FVC on choice of b/tsDMARD in RA-ILD. FVC predicts hospitalisation and mortality. However, it did not appear to influence choice of b/tsDMARD. Overall 67% of RA-ILD patients initiated TNFi, weird! @rheumnow #ACR22 Abstr#245 https://t.co/swuNHv96WD https://t.co/vy5FUPnNjo

Janet Pope Janetbirdope
3 years 1 month ago
Difficult to treat #rheumatoidarthritis - phenotypes need to be defined and order of Rx may be v Impt. Well, it is really difficult @RheumNow #ACR22 session 12S127 https://t.co/x3bkUP590A


















 Poster Hall
Poster Hall